Let’s talk about varicose veins. Yes, they are unsightly – those dark, discoloured, bulging and swollen veins that appear on our legs – but the reality is, what is happening to our leg veins is more than skin deep.
It is estimated that 20 per cent of the Canadian adult population has varicose veins. While many believe the appearance of these veins are just a natural part of aging, the truth is for many they can be painful and cause discomfort, and most importantly, they can be a sign of a more serious condition called chronic venous disease.
So let’s take a look at what varicose veins are and how they develop.
What are Varicose Veins?
In short, varicose veins are twisted, enlarged veins that are a result of poor circulation.
Healthy veins play an important role in our circulatory system by returning blood delivered by our arteries back to our heart through a series of small valves that keep the blood flowing in one direction. When these valves are damaged, blood pools in these veins causing them to twist, swell and become visible.
Early signs of this damage can include itchiness and/or present as spider veins – fine blue or red blood vessels, which appear like spider webs just under the skin’s surface.
Ranging in severity, they are typically defined as veins that are dilated 4 mm in diameter. Most commonly, they appear as prominent, bulging and blue under the skin of the leg.
Beyond the visual signs, people with varicose veins can suffer from symptoms, which can include aches and feeling heaviness in the legs, burning and throbbing sensations, worsening pain when sitting or standing, and itchiness and/or discoloration around your veins.
Varicose Veins & Chronic Venous Disease
Varicose veins are typically signs most associated with chronic venous disease. A progressive condition in which vein walls and/or valves become dilated and stop working effectively, making it difficult for blood to return to the heart from the legs. Blood begins to pool and the veins become further damaged. If left untreated, chronic venous disease can lead to more serious symptoms such as blood clots and open ulcers on the leg.
There are many factors that can lead to the development of chronic venous disease, such as gender, genetics, obesity and lifestyle and occupation.
Treating Varicose Veins
Unfortunately, the only way to remove varicose veins is through procedures such as endovenous laser treatment, radio frequency ablation, sclerotherapy or stripping.The good news is that when it comes to relieving signs and symptoms of chronic venous disease like varicose veins, leg pain, sensation of heaviness and treating the underlying cause of this condition, there are options! For protection against the disease and progression, lifestyle changes, such as increased exercise, improved diet and weight loss, are a great place to start. However, these changes will not help address the underlying cause of chronic venous disease. Fortunately, there are clinically proven, over-the-counter treatments like Venixxa, which help reduce pain, lower-leg swelling and sensation of heaviness in the legs.
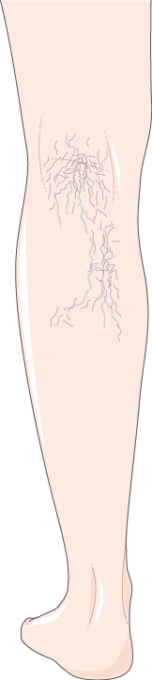
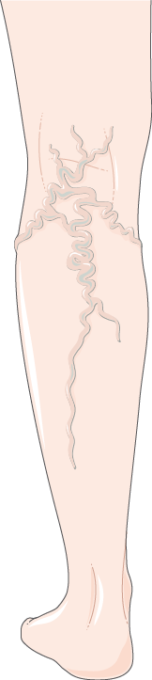

There are seven main stages of the condition from the Clinical, Etiology, Anatomy, Pathophysiology (CEAP) classification system ranging from 0 – 7. From left to right Cl: Spider Veins, C2: Varicose Veins, C7: Open Ulcer

