Chronic venous disease, sometimes known as chronic venous insufficiency, is a condition that affects the lower limbs and occurs because of poor blood circulation in the veins. In its advance stages, it can induce disabling physical and psychological pain.
Nearly 20 per cent of Canadians have experienced at least one symptom associated with chronic venous disease, yet only 30 per cent are aware of the links of their symptoms to chronic venous disease.
Symptoms are often perceived as a normal part of aging or simply an aesthetic problem.
Continue reading for more helpful information that can assist in recognizing and treating chronic venous disease in its early stages.
What causes Chronic Venous Disease?
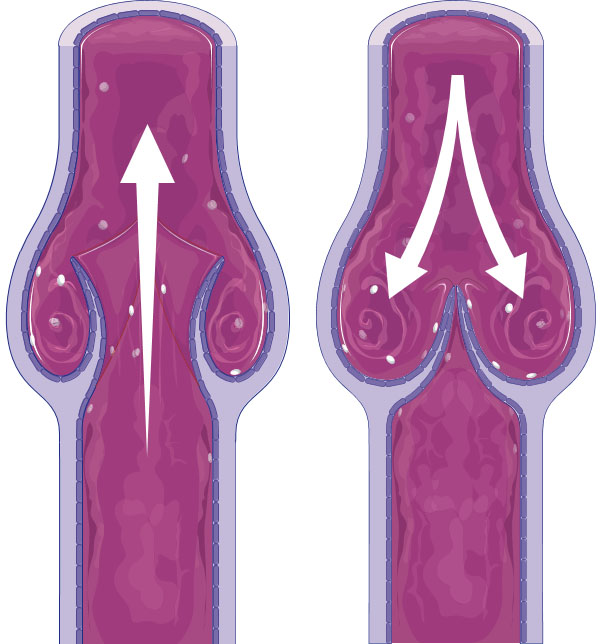
Healthy vein valves, when functioning normally, allow for one-way blood flow to the heart from all of the body’s extremities, especially when blood returns to the heart from the legs against gravity.
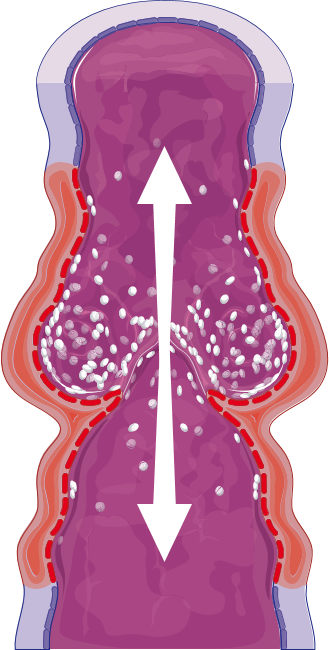
Chronic venous disease is caused by damaged vein walls and valves that are no longer working properly. As a result, blood pools in the affected veins, which damages the valves further and causes the disease to progress.
Signs and symptoms
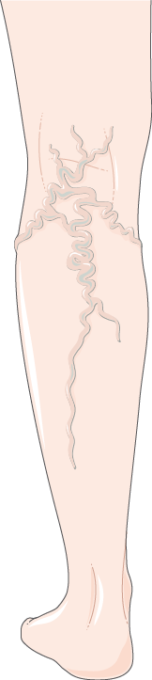
Signs and symptoms of chronic venous disease manifest in the lower limbs. They are often mistaken for signs of aging or over-exertion. Some symptoms are not visible to the eye, such as general leg pain and heavy legs, but there are also some visible signs of the disease like the appearance of varicose veins or other skin conditions in more extreme cases.
see: Expert’s advice with Dr. Chan
Chronic venous disease and varicose veins
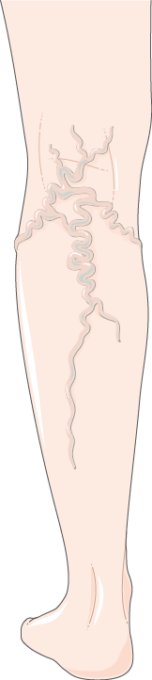
Varicose veins are one of the physical manifestations of chronic venous disease. Roughly 20 per cent of the Canadian adult population has varicose veins. While they can range considerably in severity, they are typically veins that are dilated 4 mm in diameter. Varicose veins may appear as prominent, bulging and blue under the skin of the leg, but the severity is not necessarily determined by their physical appearance.
Varicose veins are caused by the malfunction of valves within the venous system typically associated with chronic venous disease and often appear with other symptoms of the disease. Symptoms related to chronic venous disease include leg pain, itchiness or heaviness in the legs.
Once varicose veins appear, the only way to get rid of them is through medical procedures such as sclerotherapy or endovenous laser ablation. There are however ways to manage the symptoms.
Progression and prognosis of chronic venous disease
There are seven main stages of the condition from the Clinical, Etiology, Anatomy, Pathophysiology (CEAP) classification system, which is used internationally to describe and classify clinical manifestations of chronic venous disorders:
- C0 – experiencing internal symptoms (e.g. leg pain and discomfort, heaviness in the legs), but no external symptoms appearing on legs
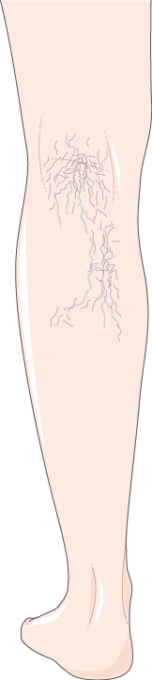
- C1 – means that spider or reticular veins are visible on legs
- C2 – means that varicose veins are visible on legs
- C3 – denotes the presence of edema (swelling) of the ankle
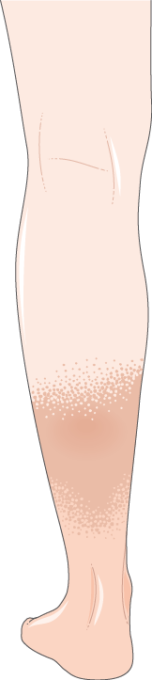
- C4 (a, b) – progression to more serious physical manifestations including pigmentation (darkening) of the skin, eczema (redness, itching), lipodermatosclerosis (hardening of the soft tissues), and atrophie blanche (whitish patches of skin)
- C5 – indicates a healed venous ulcer is present when looking at the leg

C6 – is the most severe category, indicated by an active open venous ulcer is seen on the skin

Can chronic venous disease be cured?
While there is no cure for chronic venous disease, catching and treating it early can prevent the disease from progressing further and causing irreparable damage.
Overall lifestyle modifications, including regular exercise to increase blood flow, diet change and weight loss for overweight people can help reduce symptoms of chronic venous disease.
It’s important for those living with chronic venous disease to monitor the time they spend both sitting and standing. Due to the global pandemic caused by COVID-19, routines have been disrupted and many sufferers find themselves either isolated at home or working long hours on their feet.
People who are at home should ensure they are getting regular exercise and monitoring the periods of time they spend sitting. For those who have been deemed essential workers to support their communities through the novel coronavirus crisis, it is important to be aware of the amount of time spent standing and take breaks as frequently as possible within their circumstances.
Wearing compression stockings and keeping the legs elevated to increase blood flow can also help improve the experience of those living with the disease. Compression socks or stockings that rise to the knee (versus over the knee) are more effective, as they directly target the affected area.
In addition to lifestyle modifications, topical creams and gels are popular methods used for symptom relief, but most do not address the deep-rooted issues causing chronic venous disease. Over-the-counter products, including venoactive products, relieve signs and symptoms by increasing blood flow through the veins and assist with pain management associated with the disease.
Venixxa is the number one doctor recommended over-the-counter brand to relieve symptoms of mild to moderate chronic venous disease. It works by improving venous tone, which in turn helps improve blood circulation. Venixxa is available in most drug stores and online. People looking for more information can ask their health care provider.
Assess your symptoms to know if you are at risk
If you are experiencing leg pain, leg heaviness or varicose veins, you may be at risk of chronic venous disease. Take the veinscore assessment to understand your symptoms and learn if you are at risk.

